
Psoriasis Awareness Month
August is Psoriasis awareness month, so this month’s blog will focus on how this condition affects the feet and how Podiatrists can help you manage any skin changes.
About Psoriasis
Psoriasis is a chronic skin condition, thought to be autoimmune in origin. Although it can start at any age, the most common age for onset is between 20 and 30, and 50 to 60. It is thought to affect around 1 in 50 people. It can have flare-ups and remissions.
Symptoms can vary depending on the type of the condition, but the most common types cause patches of flaky skin. These occur mainly on the knees and elbows, along with the back and scalp. It can also affect the hands and feet.
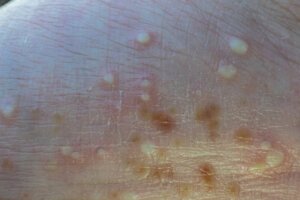
There is one type of Psoriasis that affects mainly just the hands and feet. This is called Palmoplantar Pustulosis and normally presents as reddened patches with sterile pus pockets.
Where do Podiatrists come in?
Podiatrists can help you to manage the skin changes caused by Psoriasis. It can often affect the feet and hands, causing thickened patches of skin. When it affects the palms and soles, it is known as Palmoplantar. If it affects the soles of the feet, then the patches can become painful, causing splits, or fissures, in the skin. As Podiatrists, we can help manage this change to the skin and reduce the discomfort. We would gently and carefully reduce any thickened areas, and dress any splits that have occurred. We can also advise on emollients and creams to help manage the skin.
Psoriasis and nails
Around 50% of those who have Psoriasis will have nail involvement. When it affects the nails, it can cause discoloration and thickening. We can use our skills and knowledge to consider Psoriasis as a potential cause of any nail changes. Psoriatic changes to nails can look similar to fungal infections in the nail, so it’s important to rule that out. We manage any thickening of the nails by gently reducing them with an electric file to make them more comfortable.
Psoriasis and joints
Around 1/3 of those with psoriasis will develop Psoriatic Arthritis, which causes swelling and pain in the joints. Although any joint can be affected, it is often the small joints in the hands and feet that are. The toes and fingers can develop a classic sausage-type swelling, as well as swelling around the Achilles tendon. If we have patients complaining of pain and swelling in these areas of the feet, we would consider Psoriatic Arthritis as a cause. This is one of the reasons why we take such detailed medical histories from our patients.
If you think Podiatry treatment may be of benefit to you for any reason, you can book to see us here.
Frequently Asked Questions (FAQs)
The five types of psoriatic arthritis (PsA) are:
1. Symmetric PsA: Affects the same joints on both sides of the body, similar to rheumatoid arthritis.
2. Asymmetric PsA: Affects joints on one side or different joints on each side of the body.
3. Distal Interphalangeal Predominant (DIP) PsA: Affects the small joints near the ends of the fingers and toes.
4. Spondylitis PsA: Affects the spine, causing stiffness and pain in the neck, lower back, or sacroiliac joints.
5. Arthritis Mutilans: A severe, deforming type of PsA that can lead to significant joint damage and disability.
There is no single test that confirms psoriatic arthritis (PsA), but diagnosis typically involves a combination of the following:
1. Medical History and Physical Exam: Assessing symptoms, joint swelling, skin and nail changes, and family history of psoriasis or arthritis.
2. X-rays and Imaging: Identifying joint damage, erosion, and inflammation.
3. Blood Tests: Checking for markers of inflammation (like CRP and ESR) and ruling out other types of arthritis, such as rheumatoid arthritis (by testing for rheumatoid factor and anti-CCP antibodies).
4. MRI and Ultrasound: Detecting detailed joint and soft tissue changes.
5. Skin Biopsy: Sometimes used to confirm psoriasis if the diagnosis is unclear. A rheumatologist uses these tests and evaluations to diagnose PsA accurately.
The most successful drug for psoriatic arthritis varies depending on individual response, but biologics, particularly TNF inhibitors like adalimumab (Humira), etanercept (Enbrel), and infliximab (Remicade), are often highly effective. Other effective options include IL-17 inhibitors like secukinumab (Cosentyx) and IL-12/23 inhibitors like ustekinumab (Stelara). Treatment choice should be personalized based on the patient's specific condition and response to therapy.
Anna Conway
BSc (Hons), MCPod, SRCh, PGcert Podiatry
Owner, Lead Podiatrist

